
Dr Sharania Moodley’s commute to work takes her to within spitting distance of one of the dozen or more world-class private hospitals dotted around the busy port city of Durban in South Africa’s KwaZulu-Natal province. Then it heads inland. Between Cato Ridge and Camperdown, it crosses into the uMgungundlovu district municipality, before curving northwest towards Pietermaritzburg.
It is a route well-known to veterans of the almost 90 km long Comrades Marathon, an iconic race in the world of long-distance endurance running. The Comrades changes direction every year, with the route from Durban to Pietermaritzburg known as the “up run”. When her shift ends, the down run will take Dr Moodley back home.
Dr Moodley is a neurologist and stroke champion at Grey’s Hospital, a state-run referral hospital with a history dating back to the mid-nineteenth century. It is one of just three state hospitals in the province that offer a neurological service, and the only one so far to be recognized for its stroke care quality with a WSO Angels Award. Across South Africa, only two other public hospitals have earned that distinction.
Private hospitals may be on Dr Moodley’s route to work but they’re not on her radar. “My role is in the state sector,” she says with calm emphasis. This is where she can reach the largest possible number of patients.
South Africa’s public healthcare system is short of everything including specialists. Of the country’s approximately 294 neurologists, only a small fraction work in public hospitals that provide care to 90 percent of the population. This means that while the ratio in the private sector is almost in line with the WHO recommended minimum of 100,000 patients per neurologist, the public sector has approximately one neurologist per one million patients.
This is what makes Dr Moodley’s route to work so significant.


Inviting Angels
Sharania Moodley is a Durban girl and she has always wanted to be a doctor.
When her older brother entered medical school well ahead of her, the dream began to grow roots. Like him, Sharania would attend Nelson R. Mandela Medical School at the University of KwaZulu Natal (UKZN). In her fourth year at medical school she attended a tutorial led by the legendary Prof. Pierre Bill (first head of neurology at UKZN) and was struck by his bedside manner, kindness and patience. He also made her irresistibly aware of neurology as an intellectually stimulating specialty and an exacting test of clinical acumen.
As a registrar Sharania was inspired to improve stroke care by Emeritus Professor Ahmed Iqbal Bhigjee and Professor Vinod Patel, past and current heads of neurology at Inkosi Albert Luthuli Central Hospital – a key teaching hospital for the medical school at UKZN and itself named for a liberation struggle leader and recipient of the Nobel Peace Prize.
Having been awakened to the need for improved acute stroke care in the state sector, she took careful note of the groundbreaking work by Dr Louis Kroon at Steve Biko Academic Hospital in Pretoria, and by Asst. Prof. Deanna Saylor at the University Teaching Hospital in Zambia. Sharania realized that as a neurologist she had work to do in order to seamlessly manage patients with acute stroke in her hospital.
“Stroke care is our space,” she says. If the neurology department at Grey’s Hospital didn’t have a stroke protocol, its stroke patients would not receive nationally and internationally accepted standards of care.
In January 2023, backed by the Head of Clinical Unit, neurologist Dr Ansuya Naidoo, Dr Sharania Moodley wrote an important email that would help shape the next two years. Determined that Grey’s Hospital should become stroke ready, she invited the Angels Initiative to visit her hospital.

Dr Moodley’s up run
In the Comrades Marathon, the “up run” from Durban to Pietermaritzburg has a deservedly cruel reputation. Seven infamous hills along the route turn the race into a seemingly never-ending upward slog – not unlike the attempt to create change in an underfunded, understaffed and frequently overcrowded healthcare setting. In these challenging circumstances, it helps to have a friend by your side who can offer crucial support and encouragement. Barely a week after receiving Dr Moodley’s email, Angels consultant Maxeen Murugan-Thevar signed up to be her running partner.
Having drawn up a simple standard operating procedure (SOP) for treating patients with acute stroke, Dr Moodley’s “up run” faced at least three steep hills. To reach the finish line, she would have to convince members of her own department of the urgent need to be stroke ready, convince other departments to support the project in word and deed, and convince an executive committee composed of among others the hospital CEO, medical manager, nursing manager, and quality program coordinator, to endorse implementation of the SOP and make a bed available where patients treated with thrombolysis could be monitored for 24 hours.
The third hill had seemed the most daunting, but then Dr Moodley found someone else running beside her.
The quality program coordinator had a personal story to share. Her own father had a stroke in 2020, she said at the conclusion of the meeting. He was taken to a private hospital where he received immediate care, and made a remarkable recovery.
The episode left a lasting impression of how important it was to receive care within the golden window following a stroke, and deepened her understanding of the importance of making timely care available and a priority for stroke patients in the government sector. This would vastly improve patient outcomes and reduce the burden of patient care on family members and ultimately the cost to the state.
It took a few months for the executive committee to confirm their support for Sharania’s project, and a very long year before the first qualifying patient arrived within an hour of symptom onset. But finally a male patient in his fifties arrived in the ER on what he didn’t know was the luckiest day of his life.
When news reached Maxeen’s ears that Dr Moodley’s team had successfully treated their first patient, she went to the hospital as soon as she could. She saw smiles, she could sense a new kind of team spirit, but when she went to meet the stroke survivor, the bed was empty. Grey’s Hospital’s first thrombolised stroke patient had woken up fighting fit and taken himself home.


“I celebrated within myself”
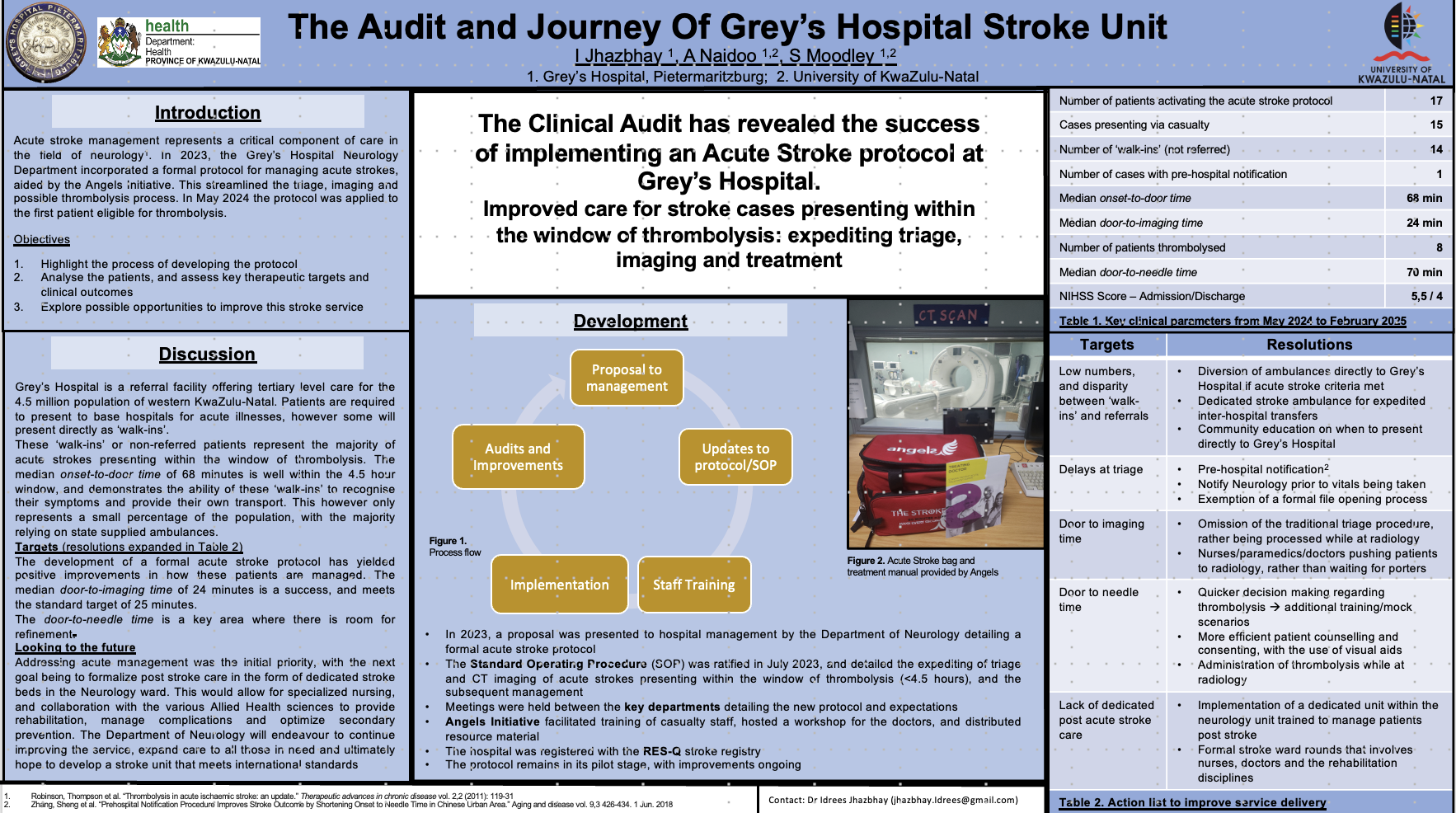
In May 2025, a poster detailing Grey’s Hospital’s stroke journey won first prize at the Congress of the Neurological Association of South Africa. By then Dr Moodley, who had added capturing stroke patient data in RES-Q to her list of tasks, already knew that Grey’s Hospital was about to write itself into the history books.
She didn’t know quite how to react to the news that Grey’s Hospital had won a WSO Angels Award. “It sounded huge, but it didn’t feel big,” she says. “I celebrated within myself as we still had yet to achieve diamond status.”
Winning the award, however rare and commendable in South Africa’s challenging public healthcare sector, didn’t mean Dr Moodley’s up run was at the end. After all, gold status in the Angels Awards only confirmed that the hospital was implementing the standard of care, as she would tell anyone who asked if the achievement was sustainable. They still had more work to do, which included a review of the post-acute phase that took most of the first half of 2025. Only then did she feel that her hospital was finally stroke ready.
If neurology registrars rotating through Grey’s decide to bite the bullet in the state system instead of being absorbed into one of the private hospital networks, at least not right away, it may be because they have witnessed a compelling example of what is possible once someone puts their mind to do something.
“We don’t have a lot but there are things we can do,” is Dr Moodley’s mantra. It rings true for both her professional and personal life. Having worked hard to earn her place in medical school, she now makes the best use of limited resources to give back to as many people as she can, as generously as she can: “I ask myself, in my short lifetime, what can I do to make the space better than I found it?”
Before Dr Moodley’s SOP for stroke care was implemented at her hospital, ambulance services in the area would bypass Grey’s if they had a suspected stroke on board. But since word got out that Grey’s didn’t just have a stroke protocol but was also an internationally recognized stroke centre, they have been known to bypass the private hospitals and – like Dr Moodley on her morning commute – set their course for Grey’s.



