In September 2018, nearly six months after I joined the Angels Initiative, I was asked to visit Pauls Stradiņš Clinical University Hospital in Riga, Latvia, to help conduct a simulation, writes Rafael Klavert, Angels Senior Coordinator.
In September 2018, nearly six months after I joined the Angels Initiative, I was asked to visit Pauls Stradiņš Clinical University Hospital in Riga, Latvia, to help conduct a simulation.
Finally, I thought to myself. Up to that point, I had been involved in various supporting roles for the European Angels consultants. However, as I am based in Germany, opportunity to visit hospitals were slightly limited. I knew it was crucial for me to experience the consultation process firsthand, so I jumped at the opportunity.
Despite having never been visited by an Angels Consultant, the hospital’s neurology department was not unfamiliar with the Angels Initiative. Just a couple months before the visit, they had already sent a couple of their young neurologists to our train-the-trainer program in Wiesbaden, Germany. And further prior to that, the hospital had also received an Angels-ESO Gold Award. Needless to say, not only were they considered a stroke-ready hospital, but also a good performing one at that.
That was when doubt started to creep into my mind. It seemed to me that they were already on the right track. How much improvement can we possibly induce from this visit? Would they find our presence useful? Or would we simply be wasting their precious time?
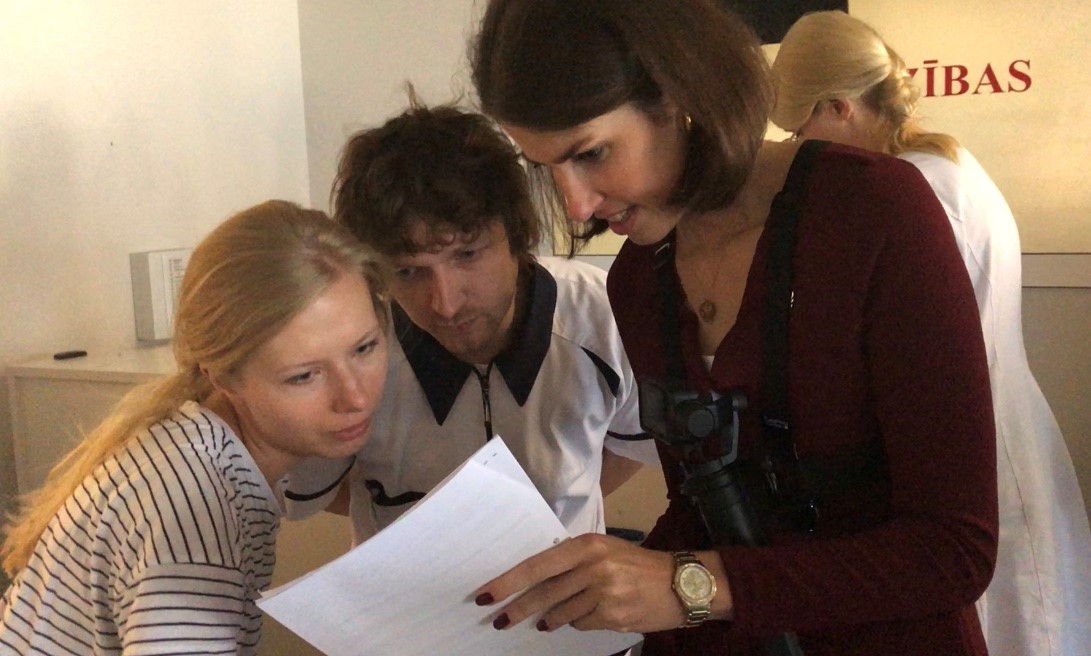
Those worries went away when we were greeted enthusiastically by Associate Professor Neurology Evija Miglane, and her group of young neurologists. I was touched to see that some of them were wearing the Angels pin. After a brief exchange of information about Angels Initiative and the state of stroke care in Latvia, we were handed over to Dr. Kristaps Jurjans, a young, tall and cheerful neurologist for a tour of the hospital, during which he proudly showed the ESO-Angels Gold Certificate framed right outside the stroke unit. “We will definitely get the Platinum status by the next reporting period”, he said with a confident smile. He also showed us the Angels Stroke Bag which he said had made things so much more efficient as everything needed to treat a stroke patient is readily available there.
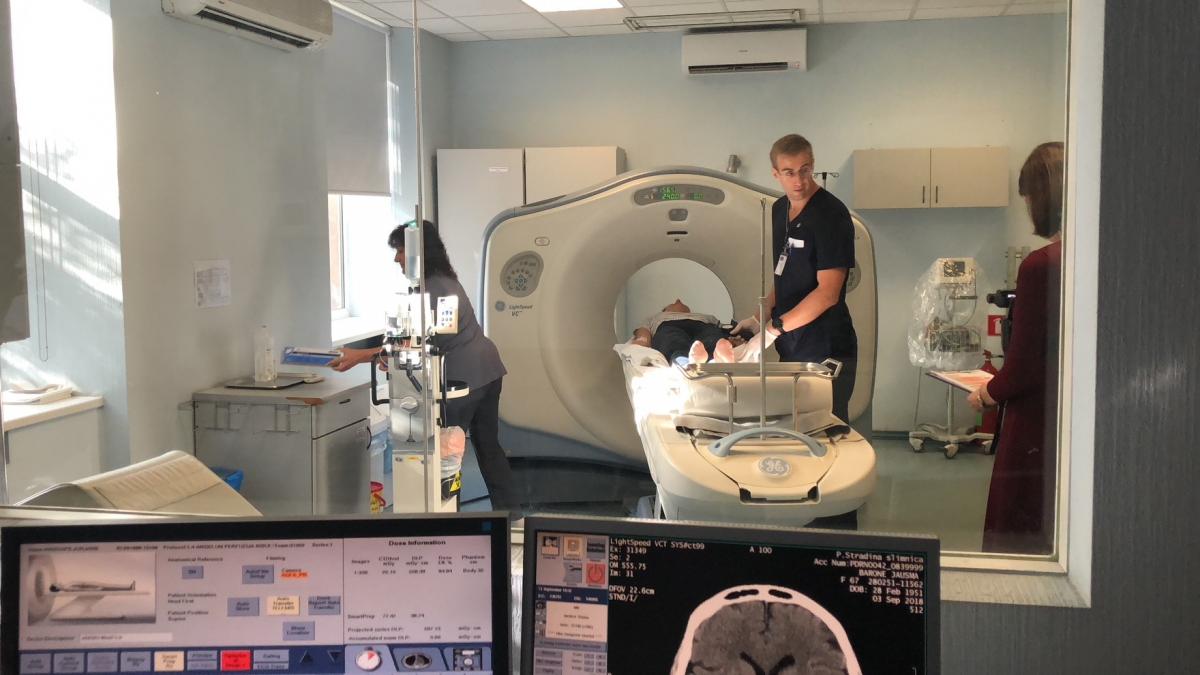
We returned the next day in order to allow time for two simulations (thankfully so, because I accidentally ripped a BIG hole on my pants during the hospital tour!). Unfortunately, we were not able to get an ambulance team to join the simulation, but there was no shortage of volunteers for that role as well as for the dummy patient role. Dr. Jurjans noted that we will be using a CT scanner that was out of service located right next to the standard CT room, so as not to disturb real patients and emergencies. You must respect someone as forward thinking and patient-oriented like that.
Once the briefings were done, we began the simulation case and it immediately became clear to me this was a well-oiled, experienced stroke team. Gone were the smiles and jokes off Dr. Jurjans’ mouth, replaced by the confidence befitting of a team leader. The first case was resolved within 20 minutes – a very impressive result by any measure, one which most hospitals and stroke teams would be proud of. But not this stroke team.

The whole process was recorded using a GoPro camera, so we regrouped with the whole neurology department to review the footage to analyze together how the pathway could be improved. Having noted that it took us nearly 10 minutes to deliver the patient to the CT, which was due to the hospital admission process as well as the distance between the emergency room and the CT room, we decided to test how much time can be saved if the ambulance team – with a hypothetical prenotification system – were to deliver the patient directly to the stroke team at the building where the CT scanner is located.
Sure enough, that little difference made a massive impact; the second dummy patient was treated within 9 lightning-quick minutes!
I was elated and couldn’t wait to review the video together, but suddenly, a real patient arrived. As the core team went to attend that emergency, we were later informed that the patient received a thrombectomy with a door-to-treatment time of 20 minutes – a verification of the stroke team’s first simulation versus real-life performance.
As I was leaving the hospital, two distinct thoughts dominated my mind. Firstly, the realization that, with the right mindset, there is always room for improvement no matter how good the benchmark had been. Secondly, yeah, they will probably reach the ESO-Angels Platinum or Diamond status in the near future.